神經回饋改善憂鬱情緒
神經回饋改善憂鬱情緒
您看過控制腦波可以驅動機器手臂泡咖啡嗎?您看過控制腦波可驅動電腦遊戲得到分數?隨著多媒體科技與神經科學的進展,許多研究證實,訓練大腦可以改善憂鬱情緒,神經回饋成為臨床心理治療新寵兒。
一、什麼是神經回饋?
神經回饋又稱大腦腦波訓練,為結合多媒體電腦科技與心理治療之非侵入性的介入模式,首先會測量個案頭皮表面的腦波訊號,透過即時的腦波訊號處理,轉換為視覺或聽覺訊息回饋給個案,治療師引導個案提升或調降某個大腦位置的腦波頻段,以達到提升專注力、降低負向情緒,改善臨床症狀之療效。
二、憂鬱症可能是調節情緒腦區不活化或過度活化
Davidson (1998) 提出前額葉alpha不對稱(frontal alpha asymmetry) 可能是憂鬱症的生物標誌,左前額葉為負責調控正向情緒的大腦,若當左前額葉的活性太低(左前額的alpha高於右前額),可能無法活化正向情緒,產生憂鬱情緒、逃避行為等現象。
本研究團隊與高雄醫學大學附設醫院與小港醫院精神科合作,在高雄地區測量憂鬱症患者與健康成年人的腦波,結果發現憂鬱症患者在大腦表層與深層呈現大腦過度活化現象(Lin, Chen et al., 2021; Lin, Yu et al., 2021),部份患者有前額葉alpha不對稱現象。因此,本研究團隊針對憂鬱症患者規劃二種神經回饋訓練方案 (圖一):
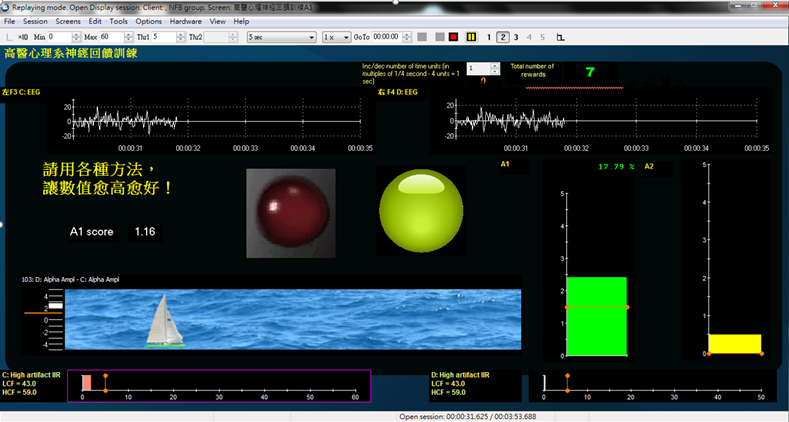
1.提升快樂腦波神經回饋 (ALAY組),以改善前額葉alpha不對稱現象:憂鬱症患者嘗試透過各種策略 (例如:回憶正向生活事件) 來提升左前額葉活性,亦即降低左前額alpha或提升右前額alpha,會使螢幕中A1分數增加(A1 = F4 alpha – F3 alpha),若A1分數大於0,且越來高越高時,電腦螢幕中連結A1分數的小船會往前移動;若提升左前額葉活性的A1分數可維持高於設定閾值的時間(例如:250或500毫秒),綠燈會亮起,給予個案視覺回饋做為獎勵。
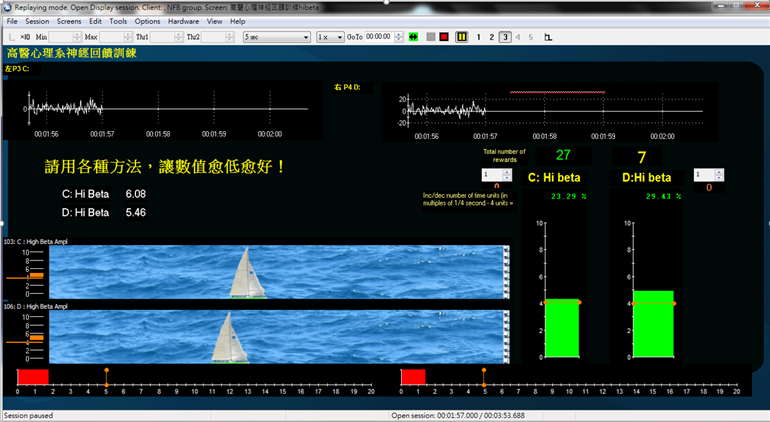
2.降低大腦過度活化神經回饋(降high-beta組),以降低大腦活化現象:憂鬱症患者可嘗試透過各種策略 (例如:保持平靜或心如止水) 來降低頂葉大腦活性,亦即降低左頂葉 (P3) 與右頂葉 (P4) 的high-beta,電腦螢幕中連結左頂葉high-beta (C) 與右頂葉high-beta (D) 的小船會靜止在水平面中;若降低high-beta數值低於設定閾值的時間(例如:250或500毫秒),綠燈會亮起,給予個案視覺回饋做為獎勵。
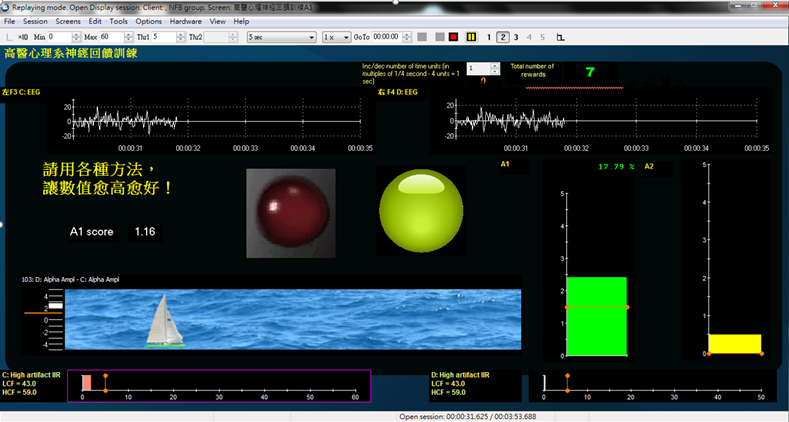
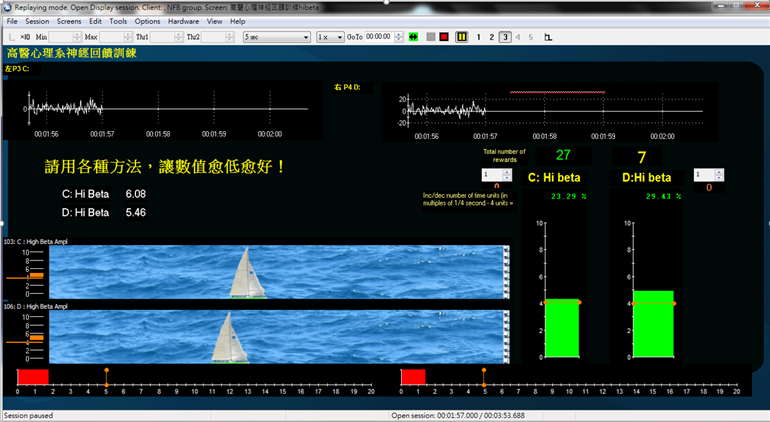
圖一、ALAY組(上圖)與降high-beta組(下圖)神經回饋訓練畫面
本研究以隨機方式將87位憂鬱症患者分派至ALAY組、降high-beta組,以及單純控制組,ALAY組與降high-beta組進行每週二次、每次一小時、共十次的神經回饋訓練,結果發現ALAY組與降high-beta組在後測的憂鬱與焦慮分數均顯著低於前測,兩組在後測的焦慮分數比控制組低,降high-beta組在後測的憂鬱分數的改善比控制組更好。此外,降high-beta組在後測頂葉的大腦活化(high-beta) 顯著低於前測,其中以左頂葉(P3) 降低high-beta更為明顯 (Wang, Lin et al., 2019)。因此,本研究結果支持神經回饋在改變腦波與憂鬱症狀具臨床有效性。
隨著憂鬱症人口日益增加,可將神經回饋訓練輔以臨床心理治療,讓憂鬱症患者學會主動提升情緒腦區的活性,降低大腦過度活化現象,提供臨床治療之獨特性和創新性的應用方向。
應用與亮點:
1.神經回饋奠基傳統心理治療基礎,結合多媒體高科技輔助,透過類似遊戲化模式進行大腦訓練,為臨床心理介入帶來新亮點。
2.透過多媒體電腦輔助設備進行憂鬱症的神經回饋,有助增加快樂情緒大腦活動、改善大腦過度活化現象,進而改善臨床憂鬱症狀,可做為輔助醫療的心理介入新趨勢。
【研究團隊】
團隊成員:本論文主要研究者林宜美教授
代表單位:人社院心理學系
研究聯繫Email:psyiml@gap.kmu.edu.tw
【論文資訊】
論文出處:Wang, S. Y., Lin, I. M.*, Fan, S. Y., Tsai, Y. C., Yen, C. F., Yeh, Y. C., Huang, M. F., Lee, Y., Chiu, N. M., Hung, C. F., Wang, P. W., Liu, T. L., & Lin, H. C., (2019). The effects of ALAY and high-beta down-training neurofeedback for patients with major depressive disorder and anxiety symptoms. Journal of Affective Disorders, 257, 287-296. https://doi.org/10.1016/j.jad.2019.07.026
參考文獻:Lin, I. M., Yu, H. E., Yeh, Y. C., Huang, M. F., Wu, K. T., Ke, C. L. K., Lin, P. Y., & Yen, C. F. (2021). The prefrontal lobe and posterior cingulate cortex activations in patients with major depressive disorder by using standardized weighted low-resolution electromagnetic tomography. Journal of Personalized Medicine, 11(11),1054. https://doi.org/10.3390/jpm11111054
Lin, I. M., Chen, T. C., Lin, H. Y., Wang, S. Y., Sung, J. L., & Yen, C. W. (2021). Electroencephalogram patterns in patients comorbid with major depressive disorder and anxiety symptoms: Proposing a hypothesis based on hypercortical arousal and not frontal or parietal alpha asymmetry. Journal of Affective Disorders, 282, 945-952.https://doi.org/10.1016/j.jad.2021.01.001
全文下載:https://pubmed.ncbi.nlm.nih.gov/31302517/
Neurofeedback improves depressive symptoms
Neurofeedback improves depressive symptoms
Have you ever seen a robotic arm make a cup of coffee through brainwaves? Have you ever seen paly computer game and get the points by controlling brainwaves? With the development of multimedia technology and neuroscience, many studies have confirmed that train your brain to improve depressive symptoms. Neurofeedback has become the new favorite of psychotherapy.
1. What is neurofeedback?
Neurofeedback, also known as brainwaves or electroencephalography (EEG) training, is a non-invasive intervention that combines multimedia computer technology and psychotherapy. First, the EEG signals on the scalp of the patients are measured, and the signals are converted into visual or auditory information through real-time EEG signal processing and then feedback to the patients. The therapist guides the patients to increase or decrease the EEG signals of a certain frequency band in a certain brain location to achieve the effects of improving concentration, reducing negative emotions, and improving clinical symptoms.
2. Depression may be caused by hypoactivation or hyperactivation of emotional brain regions
Davidson (1998) proposed that the frontal alpha asymmetry may be a biomarker of depression. The left prefrontal lobe is related to positive emotions. Hypoactivation in the left prefrontal lobe (the left prefrontal alpha higher than the right prefrontal alpha) may related to depression and avoidance behavior.
Our research team has cooperated with the Department of Psychiatry of the Kaohsiung Medical University Hospital and the Siaogang Hospital. We measured EEG patterns of patients with major depressive disorder (MDD) and healthy adults in Kaohsiung area (Lin et al., 2019; Lin et al., 2021), and we found some patients with brain surface and deep brain hyperactivity or frontal alpha asymmetry. Therefore, the research team plans two neurofeedback training protocols for patients with MDD (Figure 1):
(1) Neurofeedback for improving happy EEG (ALAY group) and improving the frontal alpha asymmetry: Patients with MDD try to increase the activity of the left prefrontal lobe through various strategies (e.g., recalling positive life events), that is, lowering the left prefrontal alpha or increase right prefrontal alpha, which will increase the A1 score on the screen (A1 = F4 alpha – F3 alpha). If the A1 score is greater than 0 and becomes higher and higher, the boat connected to the A1 score on the screen will move forward. If the A1 score remains above the threshold for a period of time (e.g., 250 or 500 ms), they will receive the green light on as the visual feedback.
(2) Neurofeedback for decreasing brain hyperactivity (high-beta inhibited group): Patients with MDD try to reduce the brain activity of the parietal lobe through various strategies (e.g., keep calm or keep the mind settled as still water), that is, reduce high-beta of the left (P3) and right (P4) parietal lobes. If the patients can reduce brain hyperactivity, the boat connects to P3 high-beta (C) and P4 high-beta (D) on the computer screen will be still in the horizontal plane. When the high-beta value is lowered below the threshold for a period of time (e.g., 250 or 500 ms), they will receive the green light on as the visual feedback.
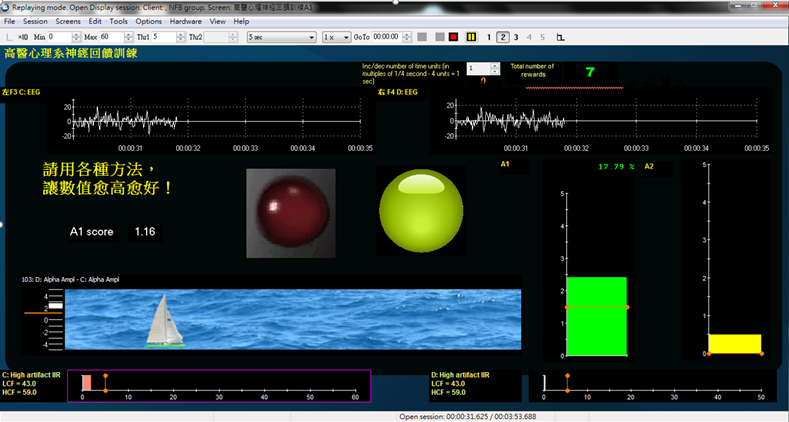
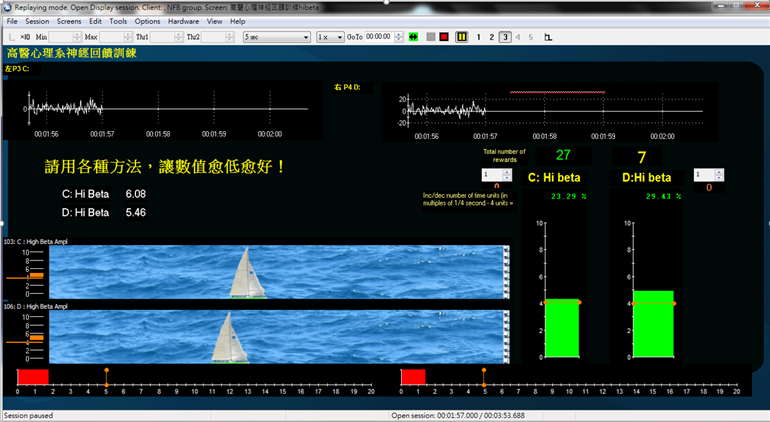
Figure 1. The neurofeedback training screens for the ALAY (above) and the high-beta inhibited (below) groups.
Eight-seven patients with MDD were randomly assigned to ALAY group, high-beta inhibited group, and control group. The ALAY and the high-beta inhibited groups underwent neurofeedback training twice a week, one hour each session, a total of ten sessions. The results found that the depression and anxiety scores in the post-test of the ALAY group and the high-beta inhibited group were significantly lower than those in the pre-test, and the anxiety scores in the post-test of the both groups were lower than those in the control group. The improvement in depression score in the high-beta inhibited group was better than that in the control group. In addition, the brain activation (high-beta) of the parietal lobe was significantly lower in the post-test in the high-beta inhibited group than that in the pre-test, especially in the left parietal lobe (P3) (Wang, Lin et al., 2019). Therefore, the results support that neurofeedback had clinical efficacy in changing brainwaves and improving depressive symptoms.
With the increasing number of patients with depression, neurofeedback training can be supplemented with clinical psychotherapy. Patients with MDD can learn to active the left positive emotional brain regions, reduce brain hyperactivity, and provide unique and innovative applications for clinical treatment.
Applications and Highlights:
(1) Neurofeedback lays the foundation for traditional psychotherapy, and combines with multimedia high-tech assistance, brain training through a game-like model, and brings new highlights to clinical psychological intervention.
(2)Through multimedia computer aids, neurofeedback can help increase happy emotional brain activity, improve brain hyperactivation, and improve clinical depressive symptoms in patients with MDD. It can be used as a new trend in psychological intervention as complementary medicine.
Research Team Members
Researcher: Professor I-Mei Lin, Department of Psychology, Kaohsiung Medical University
Contact Email: psyiml@gap.kmu.edu.tw
Publication: Wang, S. Y., Lin, I. M., Fan, S. Y., Tsai, Y. C., Yen, C. F., Yeh, Y. C., Huang, M. F., Lee, Y., Chiu, N. M., Hung, C. F., Wang, P. W., Liu, T. L., & Lin, H. C., (2019). The effects of ALAY and high-beta down-training neurofeedback for patients with major depressive disorder and anxiety symptoms. Journal of Affective Disorders, 257, 287-296. https://doi.org/10.1016/j.jad.2019.07.026
References: Lin, I. M., Yu, H. E., Yeh, Y. C., Huang, M. F., Wu, K. T., Ke, C. L. K., Lin, P. Y., & Yen, C. F. (2021). The prefrontal lobe and posterior cingulate cortex activations in patients with major depressive disorder by using standardized weighted low-resolution electromagnetic tomography. Journal of Personalized Medicine, 11(11),1054. https://doi.org/10.3390/jpm11111054
Lin, I. M., Chen, T. C., Lin, H. Y., Wang, S. Y., Sung, J. L., & Yen, C. W. (2021). Electroencephalogram patterns in patients comorbid with major depressive disorder and anxiety symptoms: Proposing a hypothesis based on hypercortical arousal and not frontal or parietal alpha asymmetry. Journal of Affective Disorders, 282, 945-952.https://doi.org/10.1016/j.jad.2021.01.001
Full-Text Article: https://pubmed.ncbi.nlm.nih.gov/31302517/