慢性C型肝炎病毒清除可減少肝外癌症發生-一大型全國多中心註冊系統研究
慢性C型肝炎病毒清除可減少肝外癌症發生-一大型全國多中心註冊系統研究
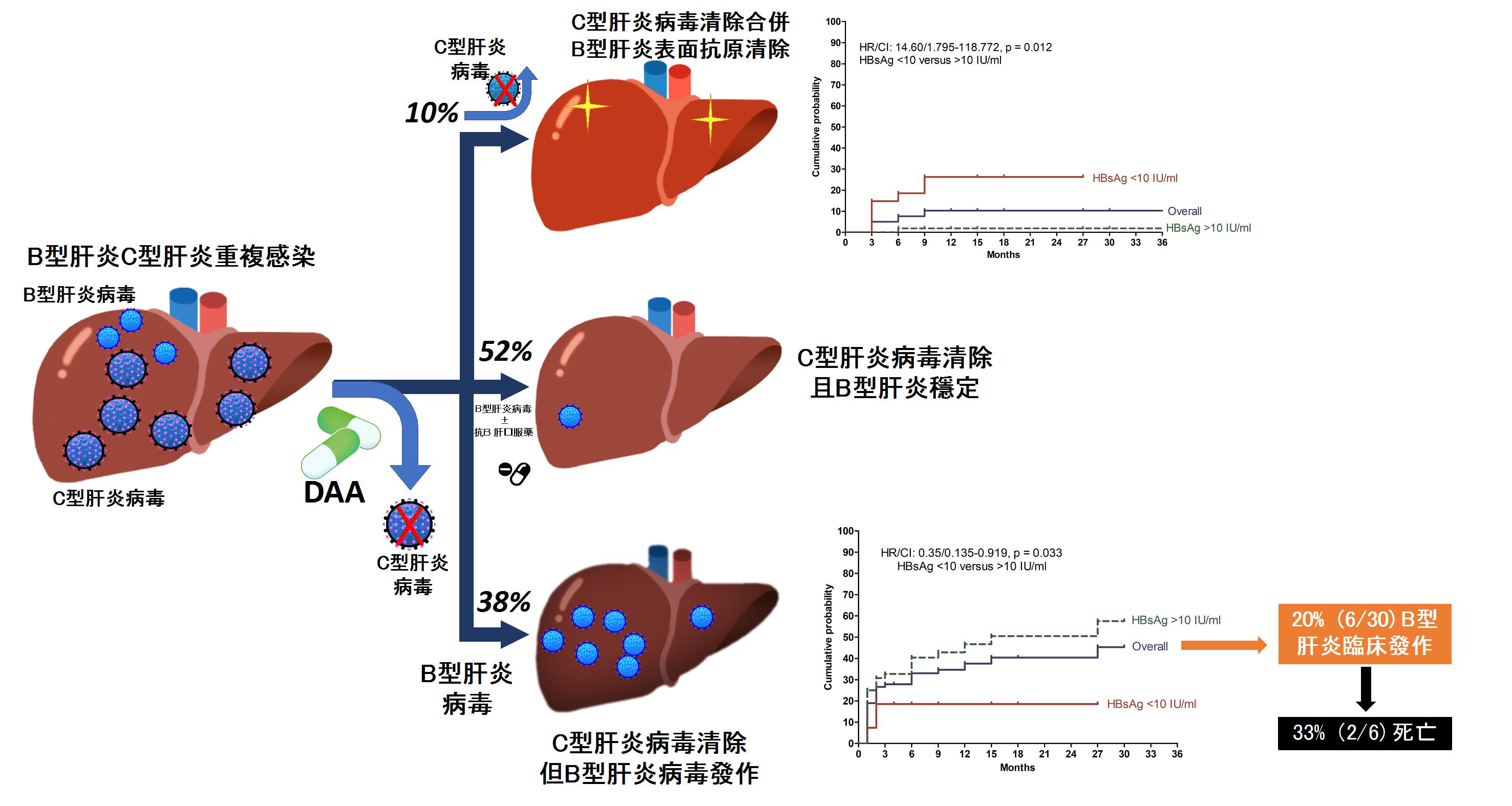
C型肝炎感染是國人僅次於B型肝炎引起肝硬化及肝癌的主因。與B型肝炎病毒不同的是,由於C型肝炎病毒具自體免疫和淋巴增生的特性,感染慢性C型肝炎有許多肝外的表徵,如增加糖尿病、心腦血管疾病、慢性腎病等風險。C型肝炎感染亦可能增加肝外癌症如淋巴癌等的發生率。成功的將C型肝炎病毒清除除了可顯著降低肝臟相關併發症風險外,也可降低肝外表現,如糖尿病發生、末期腎病等。值得注意的是,成功C型肝炎治療是否能也能降低肝外惡性腫瘤的風險是一值得探討及待解的議題。
此研究藉由全國第一個C型肝炎註冊系統T-COACH收錄包含台灣23家醫學中心及區域醫院超過10,000名慢性C型肝炎接受干擾素療程長期追蹤的真實世界報告。其最新的研究顯示成功的將C型肝炎病毒清除可同時顯著降低淋巴癌及胃癌風險。此研究成果近期將刊登在世界腸胃學頂尖期刊American College of Gastroenterology 官方雜誌American Journal of Gastroenterology。
論文第一作者黃釧峰教授針對10,714位接受干擾素為基底的慢性C型肝炎患者針對其與國人好發及過去曾經報導可能相關的12種肝外癌症進行分析。分別有8,186 位成功治療病毒清除和2,528病毒治療失敗患者在追蹤44,354人年後發現總體癌症發生率並無不同。然而進一步研究顯示相較治療失敗病毒持續存在的患者,成功將C型肝炎清除的患者有明顯較低胃癌(gastric cancer)(0.03 % vs. 0.10 % per person-year, P=0.004) 及非霍奇金氏淋巴瘤(non-Hodgkin’s lymphoma) (0.03 % vs. 0.08 % per person-year, P=0.03)的發生率。進一步分析顯示成功病毒清除對於非霍奇金氏淋巴瘤風險的降低主要在於未滿65歲相對年輕的族群(hazard ratio/95 % confidence: 3.61/ 1.17-11.16)。針對胃癌風險,在校正了幽門桿菌等其他重要危險因子後,未能成功將C型肝炎病毒清除為預測產生胃癌的獨立危險因子(hazard ratio/95 % confidence: 3.20 /1.32-7.76)。進一步分析顯示成功病毒清除對於胃癌風險的降低亦僅限於未滿65歲相對年輕的族群(hazard ratio/95 % confidence: 3.29/1.21-8.97)及未受幽門桿菌桿菌感染的患者(hazard ratio/95 % confidence:3.07/1.19-7.94, P=0.02)。總結來說成功將C型肝炎清除可在年輕族群降低非霍奇金氏淋巴瘤及胃癌近7成之風險。因此對於C型肝炎治療應該越早越好,除了可減少肝臟相關併發症如肝硬化肝癌外,也可進一步降低肝外惡性腫瘤風險。
圖形摘要
應用與亮點:
1藉由抗病毒藥物治療使C型肝炎病毒成功的清除除了可降肝癌風險,也可減少肝外癌症的發生率。
2.C型肝炎病毒成功的清除可降低73%非霍奇金氏淋巴瘤的風險
3.C型肝炎病毒成功的清除可降低67%胃癌的風險
4.這些風險降低皆在相對年輕的病人族群較能看到好處。暗示C型肝炎患者應及早及時接受治療。
【研究團隊】
團隊成員:黃釧峰、余明隆、莊萬龍、戴嘉言、黃志富、葉明倫
代表單位:肝膽胰內科
團隊簡介:1985高醫附院內科部正式分設肝膽胰專科,為台灣第一個肝膽胰專科。除了在學術研究上,在國內肝臟醫學界扮演舉足輕重的角色。於臨床醫療服務亦多次獲得國家品質標章。科內成員亦獲醫療奉獻獎、高雄市高杏獎等服務獎章。除了附設醫院、小港醫院、大同醫院及旗津醫院之門診、病房常規服務外,亦秉持擴大服務層面之宗旨,積極參與山地原住民醫療服務、部立屏東醫院、部立旗山醫院及高雄市偏鄉及離島衛生所等支援醫療,熱心投入各種社區篩檢、義診及肝病防治推廣等服務工作。提供南台灣肝病最佳醫療服務。
研究聯繫Email:fengcheerup@gmail.com
【論文資訊】
論文出處:Am J Gastroenterol. 2020 Aug; 115(8):1226-1235.
全文下載:https://journals.lww.com/ajg/Fulltext/2020/08000/Extrahepatic_Malignancy_Among_Patients_With.21.aspx