問題導向學習於護理教育之果效:系統性文獻回顧及統合分析
問題導向學習於護理教育之果效:系統性文獻回顧及統合分析
背景/研究目的:
護理人員在醫療環境中扮演著最重要的角色之一。為因應當今快速變化和資訊爆炸的醫療環境,護理教育必須培養學生發展批判性思考能力,並具備靈活、個別化和特殊情境的問題解決能力;問題導向學習(Problem-based learning, PBL)就是其中的一種教學策略。它是一種以學生為中心的教學方法和策略,這種教學方式能使學生積極參與,並與同儕在小組中互動,確定學習目標,進行自主學習、討論和應用新的知識,且在學習過程中整合各項資源;如此可提升學生自主學習、自信心、團隊合作和溝通以及批判性思考能力。因此,本研究以系統性文獻回顧及統合分析方法,搜尋七大學術研究資料庫,針對PBL於護理教育之成效的相關研究進行剖析。
研究方法:
以統合分析法獲得護生對PBL學習成果的扼要結論。我們採用族群(Population)、介入(Intervention)、比較 (Comparison)、結果(Outcomes)和研究(Study: PICOS)作為建立標準的參考依據;參與族群為護理學生,主要以PBL為介入的研究成果,這些學術研究採用準實驗設計或隨機對照試驗設計,並以英文發表。
資料來源/文獻回顧:
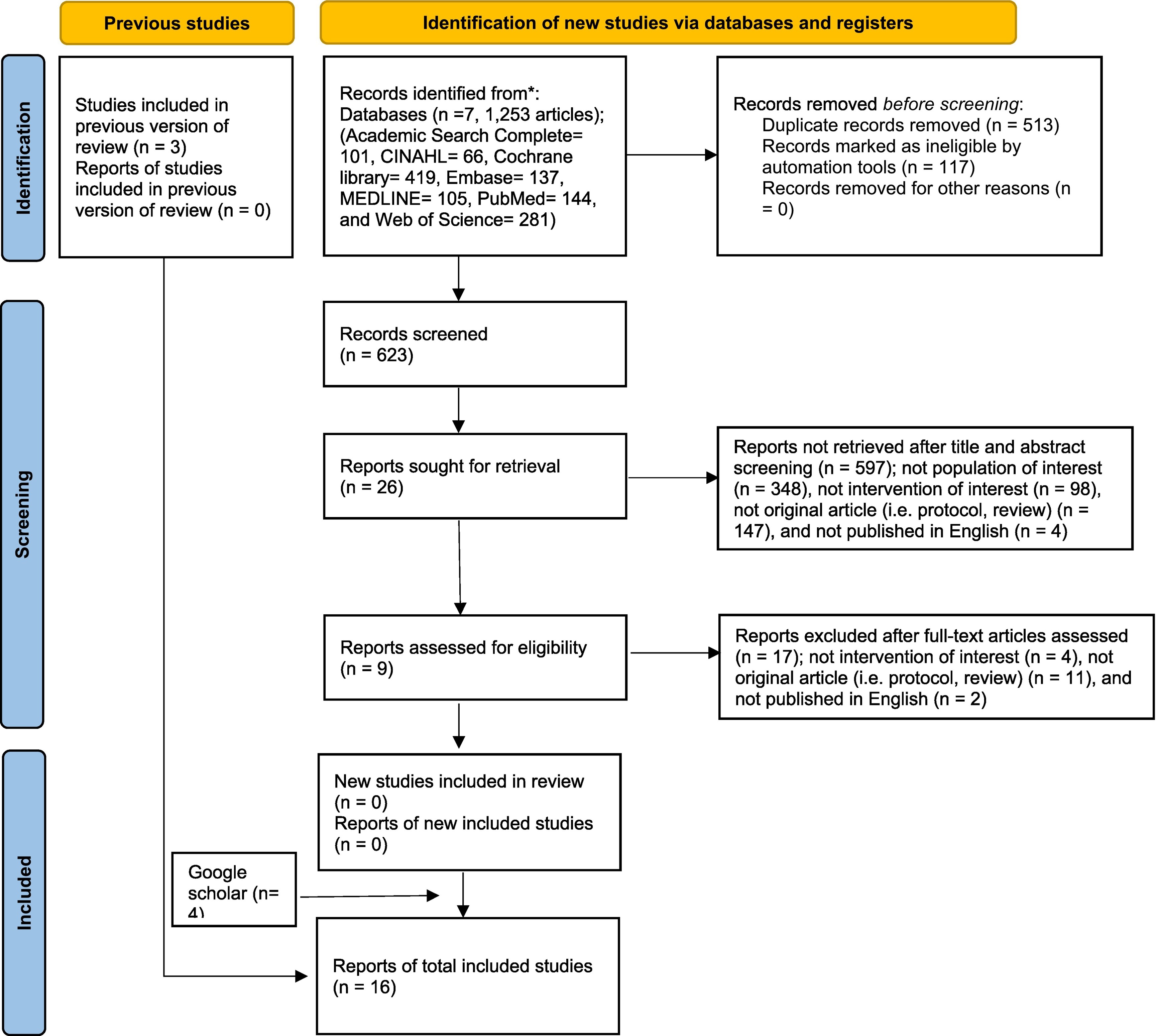
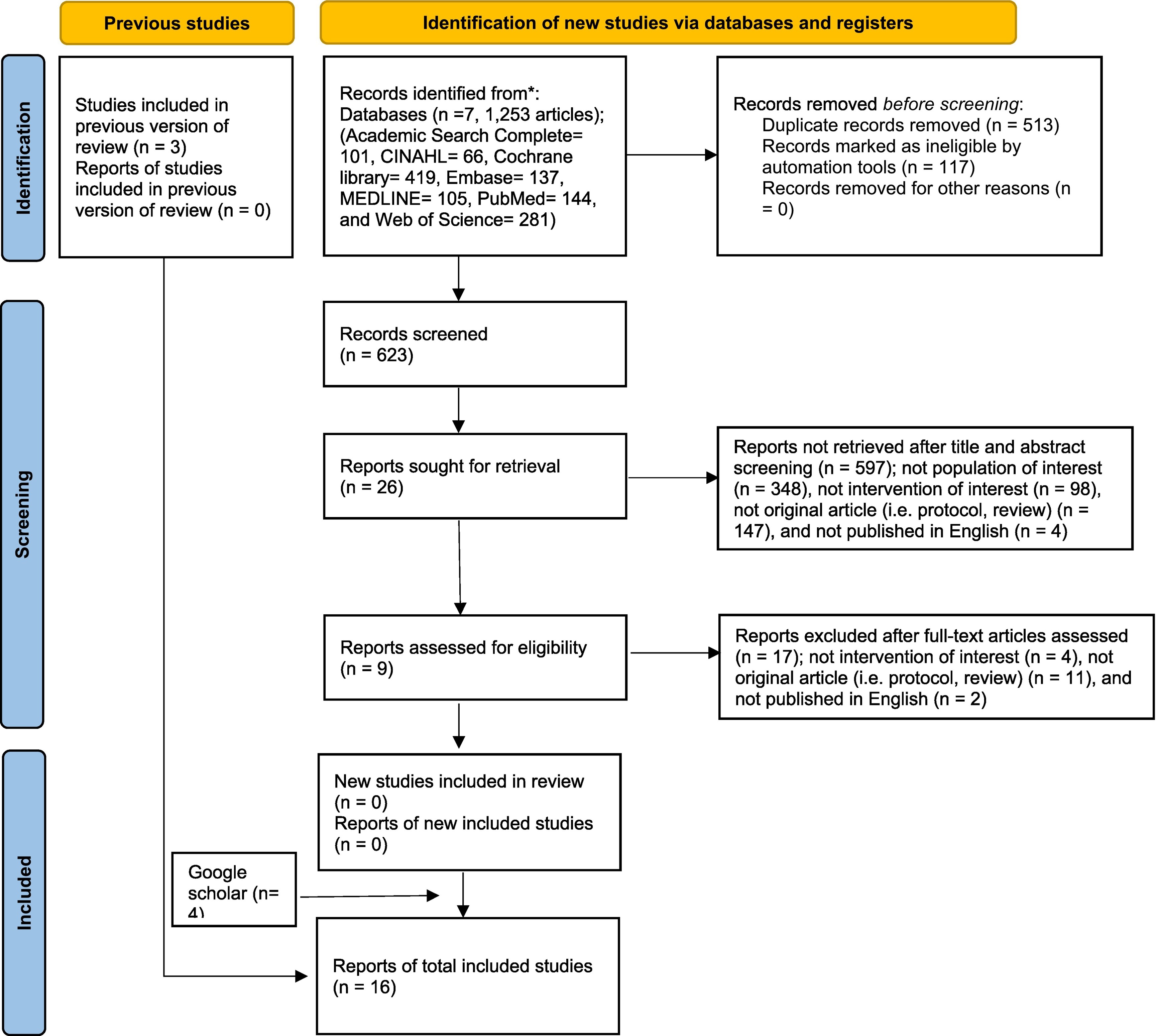
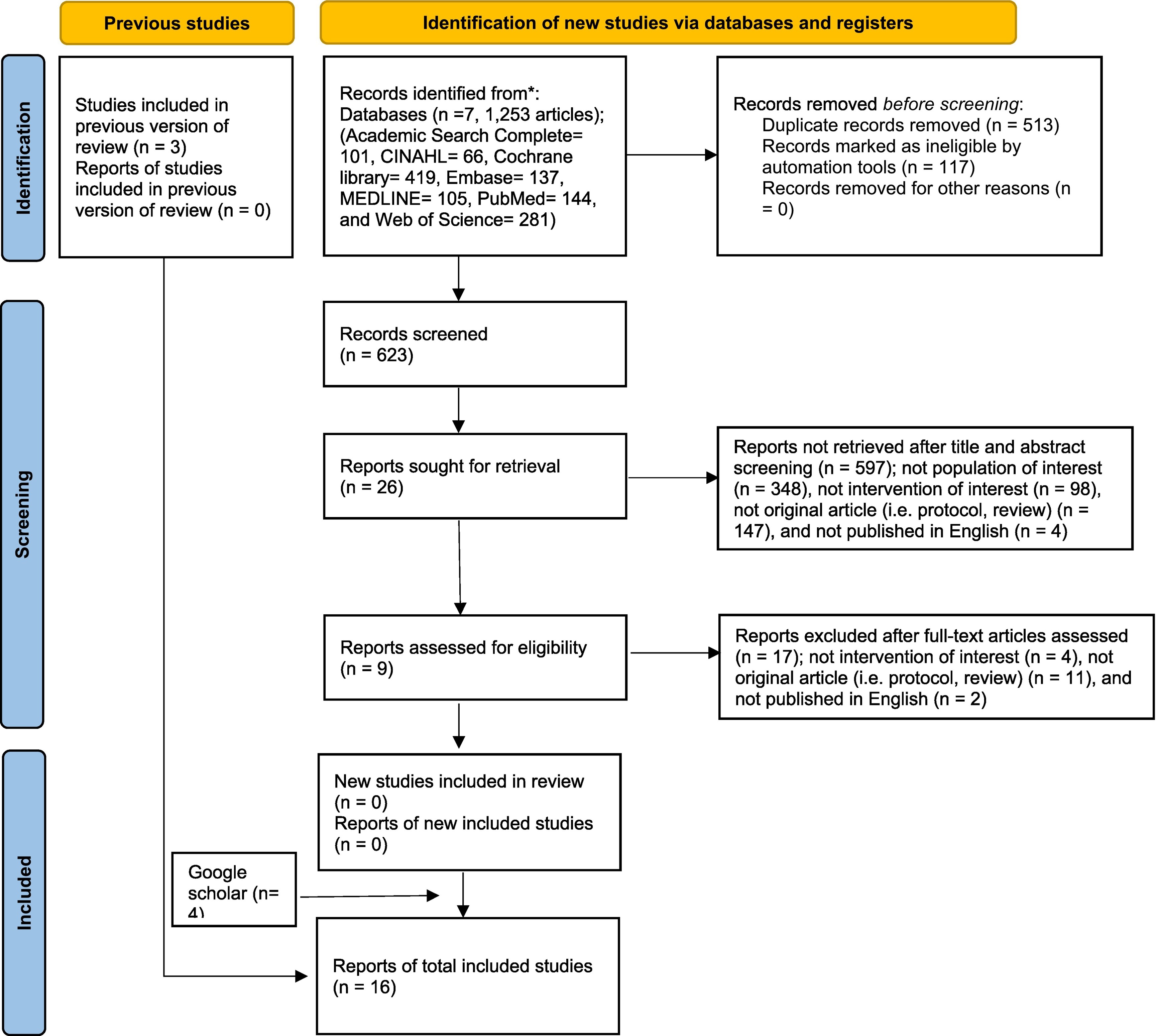
我們搜尋初始至2022年3月3日期間Academic Search Complete、 CINAHL、Cochrane Library、EMBASE、MEDLINE、PubMed以及Web of Science等資料庫共1253篇的研究發表,最後篩選完成16篇。
統計分析:
針對批判性思考能力、問題解決能力和自信心等三變項,使用隨機效應模式推估合併標準化後的平均數差異。
結果:
整體而言,在批判性思考(SMD:0.44;95% CI:0.14-0.73)、分析(SMD:0.72;95% CI:0.84-1.25)以及評鑑(SMD:0.33;95% CI:0.14-0.73)方面來說,PBL比傳統式學習有較正向的果效。然而,PBL 在問題解決和自信心變項的影響性則需要更進一步的調查研究。因此,本研究發現PBL可以增進護生的批判性思考能力,尤其在分析和評鑑方面,而此研究發現可做為未來PBL於增進學生批判性思考較傳統學習更為有效的實證依據。
圖形摘要
應用與亮點:
1.本研究發現,PBL可以增進學生批判性思考能力,尤其在分析和評鑑方面。
2.良好設計的PBL教學能有效提升護理教育中的批判性思考能力。
3.本研究雖推得PBL比傳統式學習有較正向的果效,但在問題解決和自信心變項的影響性則需要更多的調查研究。
4.針對PBL的其他潛在果效(如改善溝通技巧、學習滿意度、統合認知和自我導向學習)之更嚴格的隨機對照試驗仍是必要的;此外,PBL在護理教育長期影響也是值得進行的研究調查。
研究團隊:Sapna Sharma、Ita Daryanti Saragih、Dame Elysabeth Tuty Arna Uly Tarihoran、周汎澔
代表單位:高雄醫學大學護理學系
研究聯繫Email:fanhao@kmu.edu.tw
【論文資訊】
Sharma, S., Saragih, I. D., Tarihoran, D. E. T. A. U., & Chou, F. H.* (2023). Outcomes of problem-based learning in nurse education: A systematic review and meta-analysis. Nurse Education Today, in press. doi: 10.1016/j.nedt.2022.105631 (SCI;Nursing;I.F.: 3.906;Ranking: 8/125)
全文下載:https://pubmed.ncbi.nlm.nih.gov/36427452/
Outcomes of problem-based learning in nurse education: A systematic review and meta-analysis
Outcomes of problem-based learning in nurse education: A systematic review and meta-analysis
Background / Objective:
Nurses are the most significant component of the healthcare environment. Nurses must develop critical thinking skills in order to be competent in flexible, personalized, and situation-specific problem solving in today's healthcare environment, which is marked by rapid change and ever-increasing information. Problem-based learning is one of educational strategies can be used to develop the critical thinking and problem-solving abilities of nursing students. It is a student-centered method and strategy that allows nursing students to collaborate in small groups with the goal of improving their clinical skills and cognitive capacities. It allows students to actively participate, interact with peers in small groups to define learning goals, engage in self-study, discuss and apply new knowledge, and eventually integrate a variety of material during the learning process. This teaching method also improves self-directed learning, self-confidence, teamwork, and students' communication abilities, as well as self-assessment, peer evaluation skills, critical thinking, and interpersonal skills. Therefore, this study used systematic review and meta-analysis methods to search seven academic research databases and to analyze the relevant research on the effectiveness of PBL in nursing education.
Methods:
Meta-analysis was performed to obtain summary conclusions on the influence of PBL on nursing students' learning outcomes. To construct inclusion criteria, the Population, Intervention, Comparison, Outcomes, and Study (PICOS) approach was employed. The population comprised nursing students. Trials with a PBL intervention were included; they used a quasi-experimental design or were randomized controlled trials. In addition, only studies published in the English language were included.
Data sources / Review methods:
Academic Search Complete, CINAHL, Cochrane Library, EMBASE, MEDLINE, PubMed, and Web of Science were searched for relevant studies from the period between database inception and March 3, 2022. Seven databases yielded a total of 1253 studies, and we finally obtained and examined 16 studies.
Statistical analysis:
A random-effects model was used to generate pooled standardized mean differences (SMD) for critical thinking, problem-solving, and self-confidence. The heterogeneity of each variable in the pooled estimate was determined using a random-effects model.
Results:
Overall, PBL had a greater positive effect than traditional learning on critical thinking (SMD: 0.44; 95 % CI: 0.14–0.73), analysis (SMD: 0.72; 95 % CI: 0.84–1.25), and evaluation (SMD: 0.33; 95 % CI: 0.05–0.61). However, the impact of PBL on problem-solving and self-confidence need further investigation. PBL appears to improve nursing students' critical thinking skills, especially their ability to analyze and evaluate. The findings of this study may be used as evidence of PBL being a more effective method than traditional/conventional learning techniques for increasing students' critical thinking.
Graphical Abstract
Application and Highlights:
1.PBL appears to improve nursing students' critical thinking skills, especially their ability to analyze and evaluate.
2.Well-designed PBL teaching can effectively improve critical thinking ability in nursing education.
3.Although the findings of this study indicate that PBL had a greater positive effect than traditional learning on critical thinking, the impact of PBL on problem-solving and self-confidence need further investigation.
4.More rigorous randomized controlled trials on the influence of PBL on potential outcomes (i.e., improved communication skills, learner satisfaction, metacognition, and self-directed learning) are needed. In addition, investigations on the long-term impacts of PBL in nurse education are also necessary.
Research Team Members:
Sapna Sharma, Ita Daryanti Saragih, Dame Elysabeth Tuty Arna Uly Tarihoran, Fan-Hao Chou
Representative Department:
College of Nursing, Kaohsiung Medical University, Kaohsiung City, Taiwan.
Contact Email: fanhao@kmu.edu.tw
Article information:
Sharma, S., Saragih, I. D., Tarihoran, D. E. T. A. U., & Chou, F. H.* (2023). Outcomes of problem-based learning in nurse education: A systematic review and meta-analysis. Nurse Education Today, in press. doi: 10.1016/j.nedt.2022.105631 (SCI;Nursing;I.F.: 3.906;Ranking: 8/125)
Full-Text Article: https://pubmed.ncbi.nlm.nih.gov/36427452/