Metformin reduces hepatocellular carcinoma incidence after successful antiviral therapy in patients with diabetes and chronic hepatitis C in Taiwan
Metformin reduces hepatocellular carcinoma incidence after successful antiviral therapy in patients with diabetes and chronic hepatitis C in Taiwan
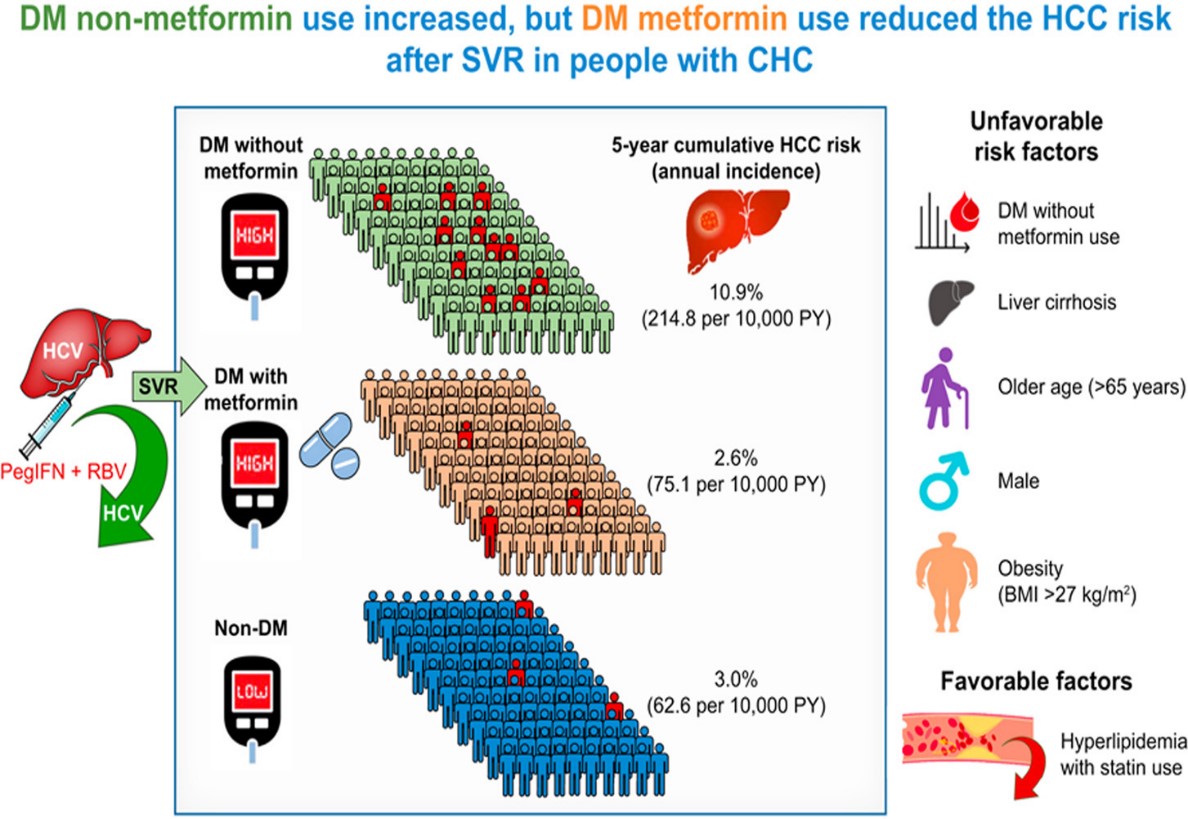
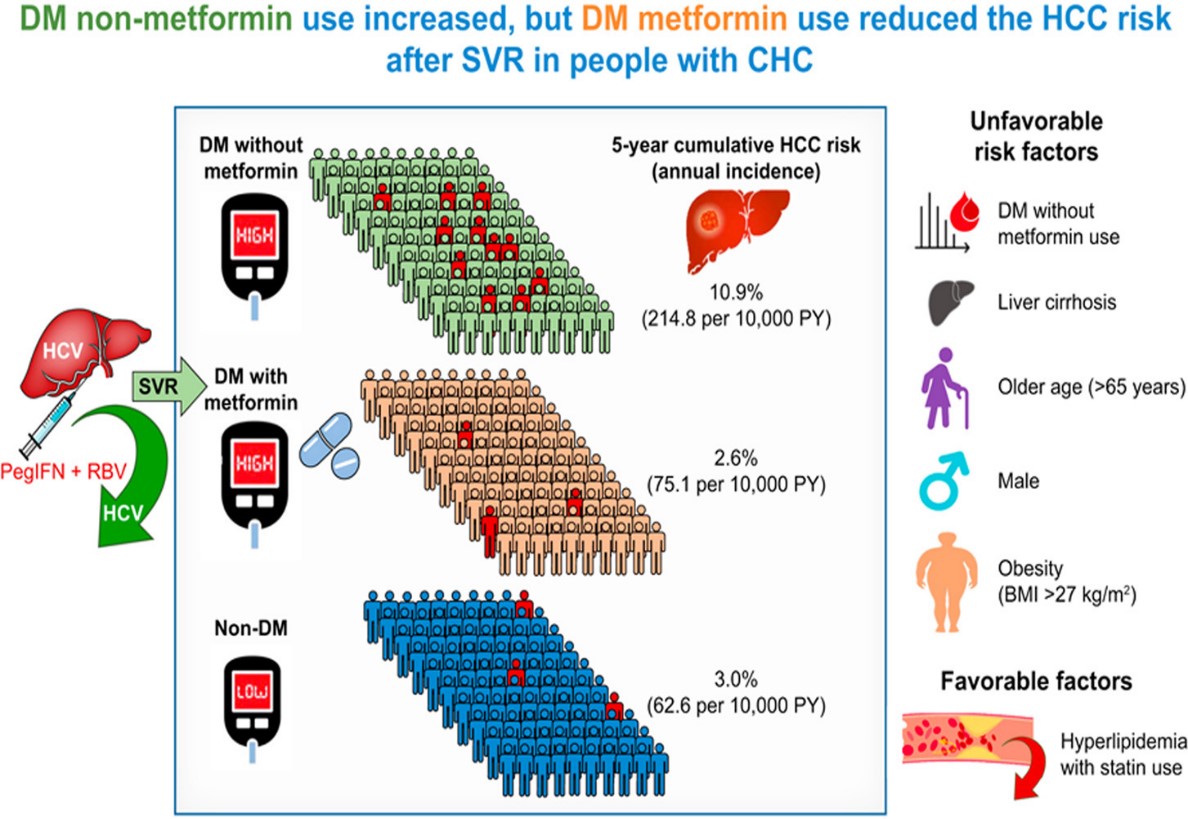
Background & aims: Diabetes mellitus (DM) is known to increase the risk of hepatocellular carcinoma (HCC) among individuals with chronic hepatitis C (CHC). Metformin is recommended as a first-line medication for DM treatment. Two systematic reviews on individuals with diabetes documented that metformin use was associated with a lower risk of HCC, and longer overall and recurrence-free survival after curative therapies for those with HCC, compared to those using other antidiabetic therapies. However, it is not known whether metformin has a role in HCC risk reduction after antiviral therapy. In this study, We aimed to evaluate whether metformin reduces HCC risk among individuals with DM and CHC after successful antiviral therapy. Methods: Individuals with CHC who achieved a sustained virological response (SVR) after interferon-based therapy were enrolled in a large-scale, multicenter cohort in Taiwan (T-COACH). Cases of HCC at least 1 year after SVR were identified through linkage to the catastrophic illness and cancer registry databases. Results: Of 7,249 individuals with CHC enrolled in the study, 781 (10.8%) had diabetes and 647 (82.8%) were metformin users. During a median follow-up of 4.4 years, 227 patients developed new-onset HCC. The 5-year cumulative HCC incidence was 10.9% in non-metformin users and 2.6% in metformin users, compared to 3.0% in individuals without DM (adjusted hazard ratio [aHR] 2.83; 95% CI 1.57-5.08 and aHR 1.46; 95% CI 0.98-2.19, respectively). Cirrhosis was the most important factor significantly associated with higher HCC risk in Cox regression analysis, followed by DM non-metformin use, older age, male sex, and obesity; whereas hyperlipidemia with statin use was associated with a lower HCC risk. Using the two most crucial risk factors, cirrhosis and DM non-metformin use, we constructed a simple risk model that could predict HCC risk among individuals with CHC after SVR. Metformin use was shown to reduce the risk of all liver-related complications. Conclusions: Metformin use greatly reduced HCC risk after successful antiviral therapy in individuals with diabetes and CHC. A simple risk stratification model comprising cirrhosis and DM non-metformin use could predict long-term outcomes in individuals with CHC after SVR.
Impact and implications: The current study provides evidence that metformin could reduce hepatocellular carcinoma (HCC) incidence after successful antiviral therapy among those with diabetes and chronic hepatitis C in a large-scale nationwide cohort study. Although successful antiviral therapy greatly reduces HCC risk in individuals with chronic hepatitis C, those with cirrhosis, diabetes, obesity, and the elderly remain at high risk of HCC development. We demonstrated that a simple risk model composed of two crucial unfavorable factors, cirrhosis and diabetes without metformin use, predicts the risk of HCC and major liver-related complications after successful antiviral therapy in individuals with chronic hepatitis C. Metformin use is highly recommended for individuals with diabetes and chronic hepatitis C after viral eradication to reduce the risk of HCC.
Graphical Abstract
Application and Highlights:
1.Diabetes mellitus is associated with an increased risk of HCC in individuals with CHC.
2.Diabetes mellitus still increases the risk of HCC after successful antiviral therapy.
3.Use of metformin for DM greatly reduces HCC risk after successful antiviral therapy.
4. A simple risk stratification model could predict the risk of HCC and other major liver-related complications.
Research Team Members:
Pei-Chien Tsai, Ming-Lung Yu, Wan-Long Chuang, Chia-Yen Dai, Jee-Fu Huang, Chung-Feng Huang, Ming-Lun Yeh
Representative Department:
Center for Liquid Biopsy and Cohort Research, Kaohsiung Medical University, and Hepatitis Research Center, College of Medicine, Kaohsiung Medical University.
Introduction of Research Team:
Professor Ming-Lung Yu are members of the Hepatitis Center and Hepatobiliary Division, Department of Internal Medicine, Kaohsiung Medical University Hospital and Hepatitis Research Center, College of Medicine, Kaohsiung Medical University, and Center for Liquid Biopsy and Cohort Research, Kaohsiung Medical University. They dedicate to the research and service of Liver diseases, including etiologies, epidemiology, pathogenesis, therapeutic modalities, and prevention of hepatitis B, hepatitis C, steatohepatitis, and liver cancers.
Contact Email: fish6069@gmail.com
Publication: J Hepatol.2023 Feb;78(2):281-292.
Full-Text Article: https://doi: 10.1016/j.jhep.2022.09.019.